Ten tips to optimize weaning and extubation success in the critically ill.
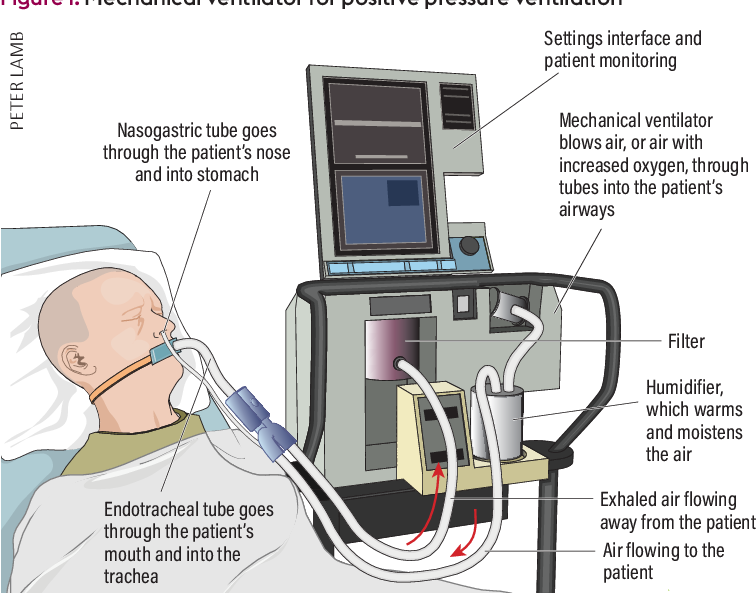
기계환기(mechanical ventilation) 치료를 받는 기간이 길어질수록 각종 합병증과 중환자실 기간이 증가한다는 것은 잘 알려져 있다. Weaning time(어떤 modality를 사용하건 간에 기계호흡으로부터 환자를 분리시키는 첫 번째 시도를 일컫는다)은 전체 기계환기 치료를 받는 기간의 50%까지 차지한다.
1. Less is more: avoid unnecessary sedation
- One cannot conceive of weaning without optimizing sedation and limiting the use of paralytics.
- Sedation protocols (nursing-protocolized targeted sedation or daily sedative interruption) have been associated with shorter duration of MV in both medical and surgical patients in comparison with no protocols, and are currently recommended by international guidelines.
진정제를 적절하게 조절하고 근이완제 사용을 제한하는 적절한 sedation protocol 사용이 필요하다.
2. Diaphragm-protective ventilation to prevent respiratory muscle complications of MV
- Prolonged controlled mode ventilation is associated with numerous complications including respiratory muscle dysfunction/atrophy, also called ventilator-induced diaphragm dysfunction, and with poor outcome.
- High tidal volumes, excessive inspiratory efforts and patient-ventilator asynchronies are associated with both lung and diaphragm injuries.
- The effort-dependent lung injury has been termed “patient self-inflicted lung injury” (PSILI)
장기간의 controlled mode ventilation은 특히 호흡근의 기능부전과 위축을 유발한다. High tidal volumes, excessive inspiratory efforts, patient-venitlator asynchony를 피해야 한다.
3. Daily screen for spontaneous breathing trial (SBT)
- To be eligible for an SBT under the European guidelines, the condition that led to the patient’s intubation must be improving and the patient’s vitals must be within physiological ranges with low or no organ support, or within acceptable limits for specific patients.
- Whether some of these items should be reconsidered remains to be tested in future studies (e.g. should we revise the classical respiratory criteria: PaO2/FiO2 > 150 mmHg, FiO2 < 40%, PEEP < 8 cmH2 O)?
환자의 상태가 호전되고 바이탈 사인이 안정적일 때 SBT를 시도한다. 하지만 SBT 시작을 결정하는 데 필요한 일부 인자에 대해서는 그 기준에 대한 재평가가 필요하다.
4. Which SBT?
- Choosing the best SBT at the bedside is not an easy task and no large study has ever compared different trials considering different clinical vignettes and respiratory physiology patterns.
- The T-Tube trial is the SBT that closely reflects post extubation inspiratory effort. However, the goal of the SBT should be, rather, to answer the question “can I wean and extubate my patient with a low risk of reintubation based on this SBT?”.
- When choosing an SBT, it is important to remember that an “easy” trial, characterized by high assistance (e.g. pressure support 7cmH2O with PEEP 5cmH20) and short duration (30 min), is associated with a higher risk of post-extubation respiratory failure than a tougher test (60–120 min of T Tube), which is associated with a higher rate of SBT failure and subsequent delayed extubation.
- This is the reason why the most recent guidelines suggest that the SBT may be performed if it has a low level of assistance and a short duration (pressure support 7cmH2O, PEEP 0cmH20, 30 min)
SBT 시 높은 수준의 support는 오히려 SBT 실패 및 delayed extubation과 관련 있으므로 낮은 수준의 support를 짧은 기간 동안 진행하는 SBT를 시행한다.
5. Protocolized or semi-automated weaning strategy
- Daily and systematic use of a checklist in a ventilator liberation protocol is associated with 25 more ventilator- free hours and one more ICU-free day compared with no protocol.
- Whether automated and semi-automated algorithms available on modern ventilators could further increase the ventilator-free days remains uncertain and may be further explored in difficult-to-wean patients.
- Similarly, proportional modes of ventilation which assist the patient by adapting to his/her effort could be considered in selected patients.
체계적인 ventilator liberation protocol을 매일 시행하는 것은 weaning에 도움이 되지만, 최신 ventilator에서 이용 가능한 automated and semi-automated algorithm, proportional modes는 좀 더 연구가 필요하며 선별된 환자에게 적용해야 한다.
6. Quickly intervene when an SBT failure
- Performing an SBT as soon as the patient becomes “eligible” should be considered as a “stress test”, both because it may shorten the duration of invasive MV and because it may unmask one or several undiagnosed conditions (with positive pressure) that should be addressed and treated before the next trial.
SBT는 positive pressure를 제공하는 동안 가려져 있던 여러 condition을 확인할 수 있는 stress test 역할도 한다.
7. Inspiratory muscle load/ force generation ratio
- SBT failure reflects an imbalance between inspiratory muscle load and neuromuscular efficiency. Because of specific muscle characteristics and load discrepancies between respiratory and limb muscle groups, the respiratory load/efficiency balance cannot be extrapolated from the examination of limb muscles.
- In patients in whom the load/efficiency balance is altered, expiratory muscles are recruited, and a better understanding of their function during acute respiratory failure has recently been highlighted.
Inspiratory muscle load와 neuromuscular efficiency 간의 불균형이 SBT failure의 주요 원인이므로 이에 대한 평가와 해결이 중요하다.
8. Weaning vs extubation failure risk factors
- Difficult-to-wean patients make up 20% of the mechanically ventilated critically ill population; being older than 65 years and being affected by cardiopulmonary comorbidities are the main known risk factors.
- Besides weaning risk factors, Jaber et al. compared the risk of airway-related vs non-airway-related risk factors for reintubation within 48 h following extubation (defined extubation failure) and reported that three risk factors were specific to airway failure (female sex, duration of ventilation > 7 days, copious secretions) and two others (non-obese status, SOFA score≥ 8) to non-airway failure.
Difficult weaning or extubation failure의 위험 인자로, 65세 이상의 고령, 심폐질환, 여성, 8일 이상의 기계호흡 치료 기간, 다량의 기관 분비물, 비만이 아닌 경우, 8점 이상의 SOFA score)를 들 수 있다.
9. Post-extubation respiratory support
- Ten to 15% of patients will need to be reintubated within 48 to 72 h post extubation.
- Standard oxygen therapy should probably be used only in easy-to- wean patients with no or few extubation failure risk factors.
- On the other hand, in high-risk patients, the combination of high-dose non invasive ventilation (NIV) (at least 12 h per day for 48 h following extubation) with high-flow nasal oxygen (HFNO) is associated with less reintubation in comparison with HFNO alone.
- In low- to moderate risk patients, prophylactic HFNO has been associated with a lower rate of reintubation than standard oxygen therapy in medical but not surgical patients.
- Likewise, HFNO is probably not inferior to NIV alone in preventing post-extubation respiratory failure and may be considered as a first- line prophylactic respiratory support option in patients with a moderate risk of weaning failure.
- In expert centers, NIV may also be used as a weaning strategy in patients who failed the SBT, as a way to provide positive pressure without the side effects of the tracheal tube and sedation.
Reintubation이 예상되는 환자에서는 extubation 후 high flow nasal cannula(optiflow)를 적용한다.
고위험 환자에서는 noninvasive ventilation을 함께 사용한다.
10. Tracheostomy
- Early vs late tracheostomy has not been associated with a better prognosis in the general ICU population versus the neurocritically ill population.
- Patients who may be considered eligible for a late tracheotomy (> 10 days of MV) are those that may benefit, for instance, from gradual weaning and constant airway/mucus plugging control.
점진적인 weaning과 지속적인 airway/mucus plugging 조절이 가능하다면 late tracheostomy(기관절개술)가 적합하다.
- Weaning and extubation success depends on careful monitoring, especially in high-risk patients, of adequate pain/sedation management, patient/ventilator interaction, and respiratory load/neuromuscular efficiency.
- A low pressure spontaneous breathing trial of short duration represents the best compromise between unnecessary prolonged MV and hazardous reintubation.
- Finally, the association between HFNO and NIV may be considered as a post-extubation respiratory support option in selected high-risk patients.
Reference
Boris Jung et al. Ten tips to optimize weaning and extubation success in the critically ill. Intensive Care Med (2020) 46:2461–2463
2024.02.26 - [의학] - 중환자에서 기관 절개술을 시행하는 시기
중환자에서 기관 절개술을 시행하는 시기
Tracheostmy Update: When and How Tracheostomy(기관 절개술)에 관한 가장 논쟁이 되는 주제 중 하나는, tracheostomy의 timing이 과연 예후에 어떤 영향을 미치는가이다. 이에 관한 많은 연구들에서 상반된 결과들
blueorbit.tistory.com
2022.05.21 - [의학] - Machine learning을 이용한 패혈증 환자의 Simple Weaning Model
Machine learning을 이용한 패혈증 환자의 Simple Weaning Model
A Simple Weaning Model Based on Interpretable Machine Learning Algorithm for Patients With Sepsis: A Research of MIMIC-IV and eICU Databases Background Invasive mechanical ventilation(침습점 기계 환기)는 sepsis(패혈증) 환자의 예후에서 중
blueorbit.tistory.com
2024.01.26 - [의학] - 기계 호흡 중인 환자에서 초음파로 흉수(pleural effusion)의 양을 측정하는 방법
기계 호흡 중인 환자에서 초음파로 흉수(pleural effusion)의 양을 측정하는 방법
Objective 본 연구는 기계 호흡을 적용 중인 환자에서 초음파를 이용하여 pleural effusion (흉수)의 양을 측정하는 방법을 알아내기 위해 진행하였습니다. Design & Setting 대학병원의 중환자실에 입원한 8
blueorbit.tistory.com
'의학' 카테고리의 다른 글
| 수술부위 감염(Surgical Site Infection) (1) | 2024.03.22 |
|---|---|
| 패혈증 환자 치료에서 과도한 수액 투여는 불량한 예후와 관련이 있다 (0) | 2024.03.22 |
| 중환자실에서 사용하는 약물 희석액의 비교 (0) | 2024.03.22 |
| Enteral nutrition(경장 영양)의 부작용 (1) | 2024.03.21 |
| Furosemide(lasix)가 급성 신손상으로 투석을 받는 중환자의 신기능 회복에 도움이 될까? (1) | 2024.03.21 |



